Original article: Poliomielite – descrizione della patologia e approfondimenti, by Ilaria Salvatori
Characteristics of the disease
Poliomyelitis, also called Polio, is a viral infection caused by Poliovirus, an enterovirus belonging to the Picornaviridae family. The term derives from the greek πολιός (poliós, gray), μυελός (myelós, marrow) with the addition of the suffix -itis (infection). It is an infection that affects the motor neurons of the anterior horns of the medulla.

Although the infection does not cause significant damage (90-95% of patients are asymptomatic), it can evolve into aseptic meningitis in 5-10% of cases. Approximately 1% of patients suffer from massive motor neuron destruction and develop a more severe form. Those with this highly disabling form experience partial or total paralysis. The most acute effects of poliomyelitis can be observed in the limbs. In addition, some subjects may develop the so-called “flaccid paralysis“: the reduced muscle stimulation leads to atrophy of the muscle, especially in the lower limbs.

How many types?
Poliomyelitis can be classified into 4 types, based on clinical features:
- Inapparent infection without symptoms;
- Abortive;
- Nonparalytic (related to the onset of aseptic meningitis);
- Paralytic.
Found in less than 1% of poliovirus infections, paralytic polio occurs when the virus enters the central nervous system. The virus can then replicate in the motor neurons of the anterior horn of the spinal cord, leading to their destruction. This form is the most disabling and, depending on the affected site, is classified into:
- Spinal: this is the most common form, and involves the motor neurons present in the anterior horns of the spinal cord. Once the motor neurons are destroyed by the virus, the muscles no longer receive adequate nerve stimulation and therefore lose their contractile capacity. This leads to muscle atrophy and total paralysis. Generally, the infection by the virus determines a situation of asymmetry for which only one of the two limbs is affected.
- Bulbar: affects the bulbar region of the brainstem, where are located important centers responsible for the control of physiological activities such as the regulation of cardiac contraction, breathing, swallowing, and metabolism. Damage of the cranial nerves (especially the glossopharyngeal nerve) and the muscles innervated by them (such as those of the soft palate and pharynx) can lead to dysphagia, dyspnea, and speech difficulties.
- Bulb-spinal: also called respiratory poliomyelitis because of the involvement of the lungs. Involvement of the phrenic nerve, which controls the movements of the diaphragm, leads to pulmonary dysfunction.
The Steel Lung
Patients whose respiratory capacity is compromised are forced to use the so-called “steel lung”, a machine that allows assisted breathing. Patients with paralysis of respiratory muscles could not be treated with oxygen alone.
Developed in 1928 by Philip Drinker and Louis Agassiz Shaw, the steel lung was a cylindrical structure connected to a pump. They created a partial vacuum that allowed air to enter the nostrils and mouth. The increase of pressure in the following phase allowed the contraction, mimicking the inspiratory-expiratory mechanism. Although this machine was highly disabling, it represented the only hope of life for many people severely affected by the disease.

Transmission
The incubation period varies from 2 to 35 days (average 10 days). The virus can be detected in the feces from 3 to 5 days following infection. During this period, the patient may be asymptomatic or present with mild flu-like symptoms such as asthenia, fever, vomiting, and headaches. Complete recovery usually occurs within 10 days.
In the more severe forms, patients experience muscle pain with breathing difficulties and heart problems. It is important to note that approximately 5-10% of severely ill patients die due to paralysis of the respiratory muscles.
Etiology and Pathogenesis
Polioviruses are transmitted from person to person as a result of excretion in feces and pharyngeal secretions. There are 3 strains responsible for the onset of the disease:
- Brunhilde or Type 1, still circulating today;
- Lansing or Type 2, declared eradicated in 2015;
- Leon or Type 3, declared eradicated in 2019.
The transmission is oro-pharyngeal: the virus can be transmitted through saliva or ingestion of contaminated water. The poliovirus enters the oropharynx and multiplies locally in the tonsils, lymph nodes in the neck, and Peyer’s plaques in the intestine. Virus entry is followed by primary viremia, which is the entry of the virus into the bloodstream after initial replication. A primary viremia can be followed by a secondary viremia, responsible for the most important effects.
The most severe forms are caused by the virus entrance within the central nervous system, but the primary access mode has not yet been identified. The most vulnerable individuals are children between 6 months and 3 years of age.
Epidemiology
Poliomyelitis is a disease with very ancient origins: the first evidence comes directly from 1300 BC. The funerary stele of the priest Rom, preserved at the Glypotek Museum in Copenhagen, depicts a man with an evident malformation of the lower limb due to atrophy caused by polio. Then, in 1789, the English physician Michael Underwood described for the first time what would be the scourge of many men and women and would lead to irreparable damage for which, even today, many individuals suffer.

The first confirmed outbreak was described in 1843 in the United States, and between the second half of the 1800s and the first half of the 1900s, America was hit hard. In particular, 1952 was a challenging year for the American population, which faced an enemy that affected approximately 60,000 children, causing more than 21,000 cases of paralysis.
Over the years, many scientists have been searching for a safe and effective polio vaccine. The real breakthrough came in 1952 when John Salk developed the first effective vaccine, and the second breakthrough came with the introduction of the Sabin vaccine in 1961.
The discovery of the polio vaccine was a real revolution as it led to a drastic reduction in incidence: the number of cases of poliomyelitis in America went from almost 58,000 to only 5,600 within a year.
What about Europe? It is estimated that, from 1961 to 1965, about 7671 children (about 74% fewer than in the early 1950s) suffered the drastic effects of polio.
Global Polio Eradication Initiative (GPEI) and current status
To permanently eradicate polio, the Global Polio Eradication Initiative (GPEI) campaign was launched in 1988, led by national governments, WHO, Rotary International, the U.S. Centers for Disease Control and Prevention (CDC), UNICEF, and other partners.
Following 1988, polio cases declined by 99%, and in the 2000s, the first significant milestones were finally achieved: in 2002, Italy was declared polio-free. A new milestone was reached last year: on August 25, 2020, the World Health Organization announced that the African continent is officially polio-free, as four years have passed since the last recorded case.
The battle against polio is not yet complete. Although Polioviruses type 2 and 3 have disappeared, type 1 persists in Afghanistan and Pakistan, where 74 cases were reported in 2015.
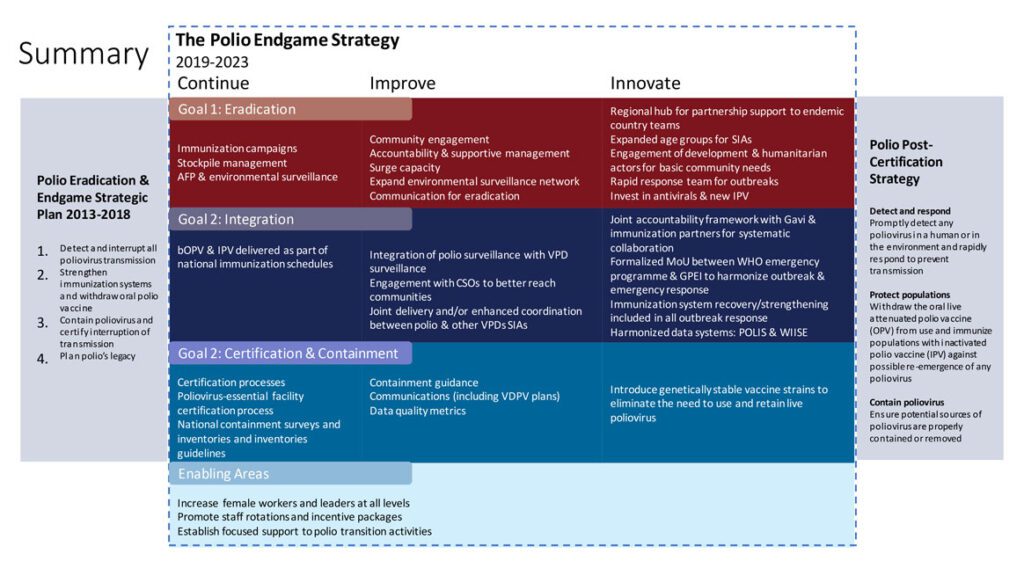
In 2019, another campaign aimed at total polio eradication had been activated: the GPEI Polio Endgame Strategy 2019-2023.
Instrumental and laboratory tests
The current method used to detect the presence of the virus is PCR (Polymerase Chain Reaction).
Isolation of the virus can occur through the use of stool samples, blood, or cerebrospinal fluid. The most commonly used samples are those of stool: the presence of the virus in stool can be detected as early as 3-5 days after infection, up to a period of 1 or 2 months. Stool samples are generally collected within two weeks after infection.
The study of cerebrospinal fluid, on the other hand, is an underused and unspecific method.
Therapy
The most important therapy is certainly prevention since there is no cure for poliomyelitis. Drug treatment with antibiotics and analgesics can be used to relieve symptoms or to prevent bacterial infection.
Currently, two types of vaccines are available: inactivated poliovirus (IVP) and oral polio vaccine (OPV).
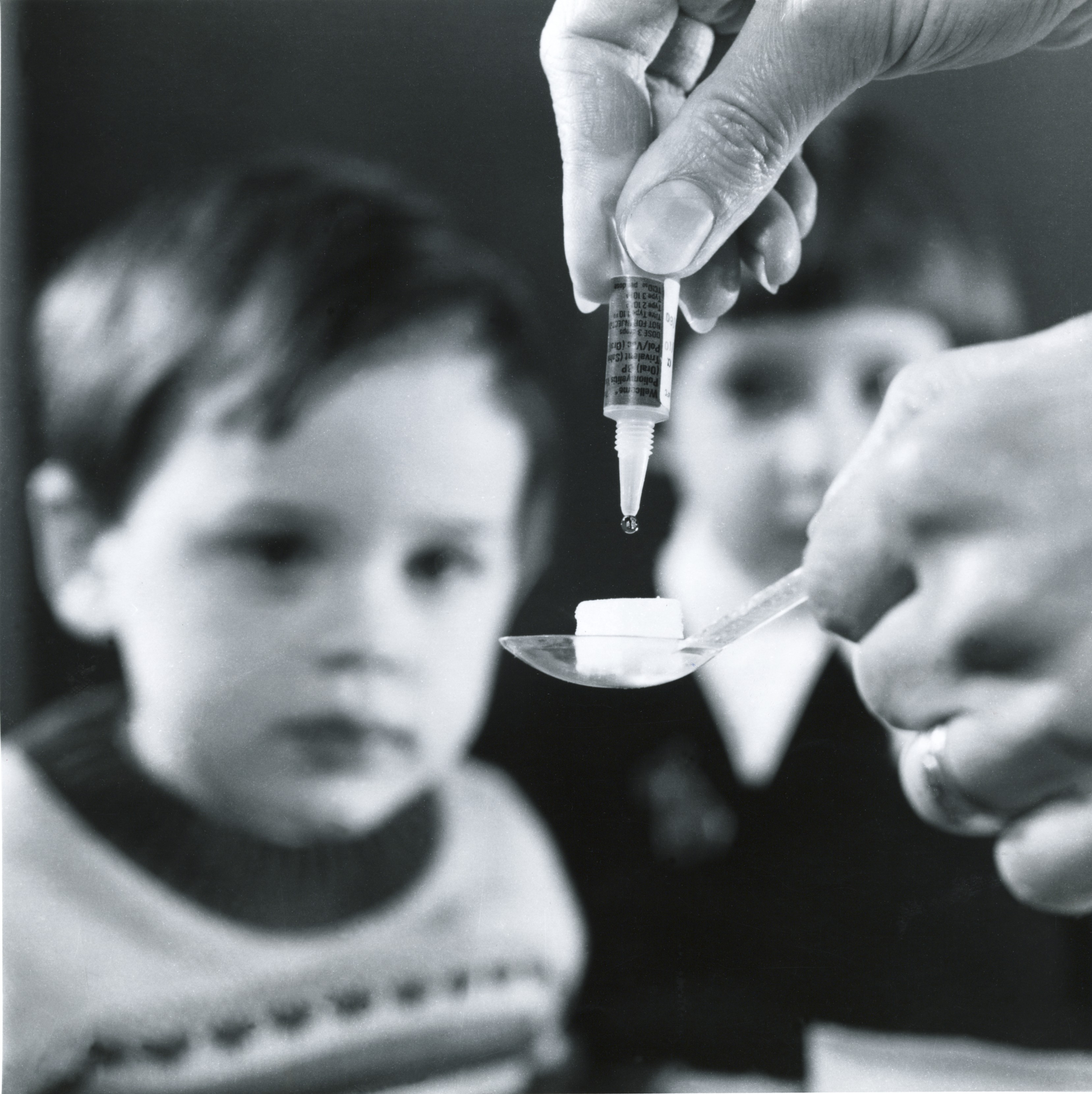
The OPV vaccine was developed by Albert Bruce Sabin in 1957 and approved in 1962. It is a live attenuated vaccine made from live microorganisms rendered non-pathogenic through specific laboratory techniques. The modifications introduced in the viral genome cause the virus to lose the ability to reach the central nervous system while maintaining the ability to replicate and activate the immune system. This type of vaccine can stimulate intestinal immunity producing immunoglobulin A (IgA), thus preventing intestinal colonization by the virus. It is an easy-to-administer vaccine; it is administered by using a small sugar cube on which is placed a drop of the vaccine.
The IVP vaccine was developed by Jonas Salk and used for the first time in 1955. It is an inactivated virus vaccine made up of a virus whose replicative capacity is lost. Therefore, it is a safer vaccine but less efficient, so it needs several recalls. In America, since 2002, the inactivated vaccine is the only one that has been approved.
Indications for the use of the IVP vaccine
Indications for proper immunization include administering 4 doses at 2 months of age, 4 months, 6 to 18 months, and 4 to 6 years of age.
For adults who have never received the polio vaccine, the protocol calls for the administration of 3 doses. The second and third doses should be administered at 1-2 months and 6-12 months after the first, respectively.
Polio vaccine is also included in the hexavalent vaccine (diphtheria, tetanus, pertussis, poliomyelitis, Haemophilus influenzae type b, and hepatitis B), which is administered in two doses at the 3rd and 5th month of life. The IPV-DTPa vaccine is used for booster around 5-6 years of age.
The problem of iatrogenic polio
One of the problems associated with the use of the OPV vaccine is the polio vaccine-induced. In some cases, especially concerning serotypes 1 and 2, the attenuated strains may mutate and develop a new virulence, causing the paralysis characteristic of polio. This event is infrequent (one case per 2.7 million doses) and is predominantly associated with those countries where polio persists. In addition, the risk of iatrogenic polio is lower for the doses following the first vaccination.
“I have had dreams, and I’ve had nightmares. I overcame the nightmares because of my dreams.” – Jonas Salk.
Ilaria Salvatori
Bibliography
- https://it.wikipedia.org/wiki/Poliomielite
- https://www.epicentro.iss.it/polio/
- https://www.msdmanuals.com/it-it/professionale/malattie-infettive/enterovirus/poliomielite
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4212416/
- https://www.who.int/biologicals/areas/vaccines/poliomyelitis/en/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2991634/
- https://www.epicentro.iss.it/polio/#:~:text=Sintomi%20iniziali%20della%20malattia%20sono,dei%20muscoli%20dell’apparato%20respiratorio.
- https://www.cdc.gov/cpr/polioviruscontainment/diseaseandvirus.htm
- http://polioeradication.org/who-we-are/polio-endgame-strategy-2019-2023/
- https://www.cdc.gov/vaccines/vpd/polio/public/index.html
- http://www.salute.gov.it/portale/vaccinazioni/dettaglioContenutiVaccinazioni.jsp?lingua=italiano&id=4802&area=vaccinazioni&menu=fasce